Intro
So much progress has been made since we shared Part I of our article series on generative AI’s potential to reshape healthcare delivery.
In this second and final part, we shift our focus from generative AI’s role in outpatient care to its potential to transform the emergency department.
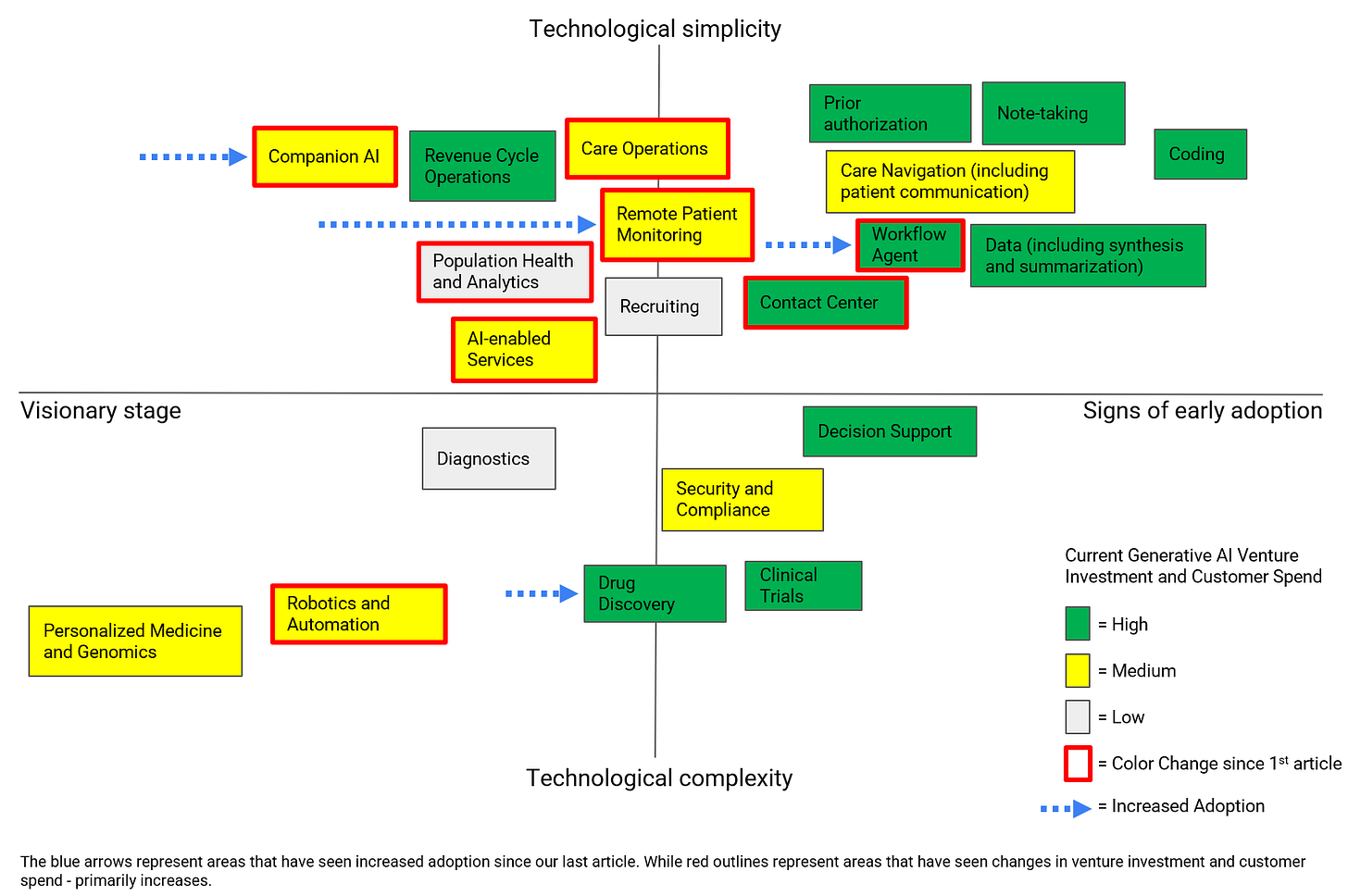
Below, we share an updated version of our 2x2. We've seen increased interest (e.g. venture dollars and customer spend) in generative AI applied to AI-enabled services, care operations, companion AI, contact centers, remote patient monitoring, robotics and automation, and workflow agents (boxes outlined in red). We've also seen increased signs of early adoption for generative AI applied to companion AI, drug discovery, remote patient monitoring, and workflow agents (arrows demonstrating this shift).
Diving Deep into the Patient Journey from a Provider’s Perspective
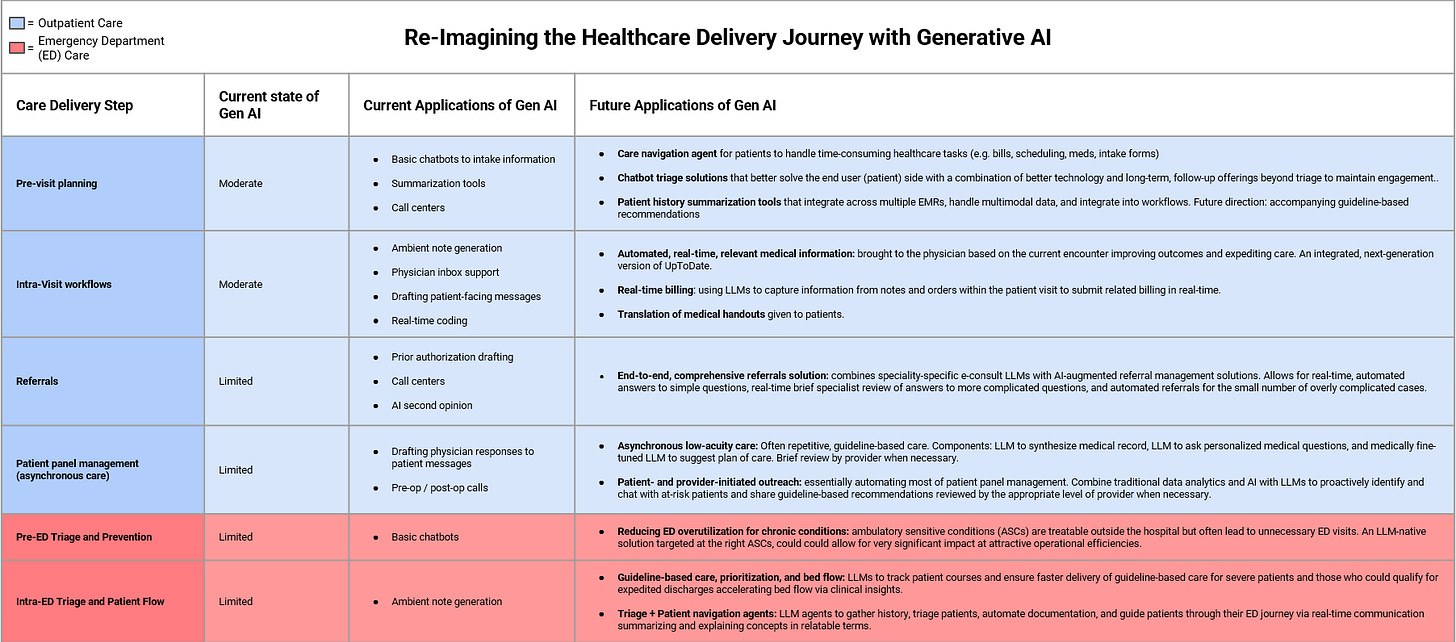
Given the early embrace of AI-driven solutions by providers, we have decided to dive deeper into this area.
Leveraging our diverse expertise in healthcare, AI, startups, and investing, our team – which includes a practicing physician – set out to break down the patient journey from a provider’s perspective for a more granular view of how AI could transform patient care.
We hope that by delving into this level of detail we can equip founders with information to spark meaningful advances in healthcare delivery.
In this report, we:
Share detailed process maps of the healthcare delivery journey
Highlight steps at which companies are already innovating and others where we think there is substantial whitespace
Discuss the LLM use cases we find most exciting and those that may be best addressed by startups
We hope that sharing this level of granularity is helpful to both seasoned healthtech veterans and to those with less healthcare experience hoping to apply their tech expertise to improving our healthcare system.
Structure
We’ve focused our care delivery analysis on what we describe as “pre-hospital” care meaning care provided to patients before being admitted to a hospital. Our first article focused on Outpatient care. This article focuses on the Emergency Department.
We have further subdivided these main sections into subsections as can be seen in the below graphic.
We will share a detailed healthcare delivery process map for each subsection and include analysis on both the steps at which AI companies currently operate and those steps at which we see lesser explored opportunities.
Emergency Department
In this article, we will focus on the emergency department, and, in our market map below, we highlight some of the companies we will discuss in this article in addition to those previously discussed in Part I.
We’ve also included two tables below: Table 1 contains the highlights for the remainder of the article and Table 2 offers guidance on what characteristics allow startups to displace incumbents using generative AI.
Table 1.
Table 2.
Pre-ED triage and Prevention
Legend:
ED = Emergency Department
PCP = Primary Care Provider
UC = Urgent Care
SNF = Skilled Nursing FacilityA Walk Through the Process Map: Pain Points, Current Solutions, and LLM Use Cases
Pre-ED Triage
The vast majority of patients will go to the Emergency Department (ED) after experiencing symptoms at home, rather than at a healthcare facility. Many of these patients will decide to visit the ED on their own, often after obtaining imperfect information from “Googling” their symptoms or searching WebMD.
Others make this decision after communicating with one of their established providers e.g. their PCP or a relevant specialist through phone calls or patient portal messages. Finally, patients are increasingly turning to ChatGPT and other similar solutions to address their health concerns.
When done right, this pre-ED triage step can add significant value to the healthcare system by reducing unnecessary ED visits since ~2/3 of visits by privately insured patients are avoidable.
There are several common reasons for unnecessary ED visits:
Not established with primary care
Inconvenient access to “on-demand” care i.e. urgent care or a patient’s own primary or specialist doctors
Patient’s misperception of the urgency of their symptoms
There are a host of solutions aimed at reducing these unnecessary ED visits, which we will discuss in chronological order from the time immediately before going to the ED to prevention months before.
911-Integrated Triage Services
MD Ally and RightSite intervene during 911 calls, the last possible moment before a patient goes to the ED. They offer 911-integrated triage service that triages patients identified as having low-acuity medical conditions to virtual care to reduce unnecessary EMS and ED usage. Subsequent patient navigator services provide value to payers by providing additional support to these patients to prevent future unnecessary ED visits: services such as prescription assistance, transportation to clinic appointments, or social services referrals.
This is an exciting space because ED diversions can be directly attributed to 911-triage solutions, which more directly demonstrates value. By contrast, other digital front door solutions that try to intercept patients earlier must make a more complex case for attribution.
We’re in the early innings of intervening here in this very promising space. In order to succeed, these companies will have to navigate through aligning incentives between payers and EMS / 911 call centers, selling through to the EMS sector, and looking ahead to what may happen next post CMS’ ET3 model’s termination in December 2023.
Chatbot Triage Solutions
Buoy and Ada were discussed in our first article’s pre-visit planning section but are very relevant again. Buoy sought to replace the typical patient “googling” behavior by connecting patients to an AI chatbot to assist with appropriate triage to reduce inappropriate ED visits. Please see our first article for more information.
Other companies include Clearstep and Fabric, who has notably been a big M&A player in the space acquiring competitors like Zipnosis and Gyant.
Home-Based Alternatives to ED
Other startups such as Dispatch Health and myLaurel offer a different solution to avoid ED visits and hospitalization by providing a spectrum of care from on-demand telemedicine services to in-person home care including urgent care and home hospital services.
Reducing ED Overutilization for Chronic Conditions
Another problem driving up healthcare costs is the overutilization of the ED for ASC (ambulatory-sensitive conditions) i.e. conditions that should be treatable outside of the hospital. Several common chronic ASC conditions that lead to preventable ED visits and hospitalizations include: heart failure, chronic obstructive pulmonary disease (COPD), asthma, and musculoskeletal conditions (MSK) e.g. back pain.
Several companies are targeting excessive healthcare use, including ED visits, across these conditions: Story Health for heart failure, Karoo Health and Heartbeat Health partnering to deliver general cardiology value-based care with Chamber Cardio also in the space, Ansible Health and Propeller Health for COPD and asthma, and Sword Health, Hinge Health, and Vori Health for MSK issues. Some of these companies have been acquired (Propeller Health acq. by ResMed) or achieved unicorn valuations (e.g. Sword Health, Hinge Health) reflecting the significant value they provide. These firms vary in their focus areas e.g. MSK startups primarily aim to cut back on unnecessary imaging and surgeries, which has also led to fewer ED visits.
Companies like Hinge Health are already using LLMs to better personalize messaging to patients in the hopes of increasing engagement and outcomes:
“Our communication with members often involves asynchronous messaging, which is greatly enhanced by LLMs. These models integrate various information sources and previous interactions to create draft messages that are not only time-efficient but also highly personalized and context-rich. To build trust and adoption among our care team, we focus on the transparency of LLMs, showing the reasoning behind each message. This approach combines the strengths of AI and human input, allowing our team to quickly edit and further tailor messages. Our goal isn't just cost-saving; it's to improve member engagement and satisfaction, and clinical outcomes, while maintaining our clinical costs." — Gabriel Mecklenburg, Co-founder & Executive Chairman of Hinge Health
The Agency for Healthcare Research and Quality has compiled a list of the top 20 most frequent diagnoses for treat-and-release ED visits. These types of ED visits are often either preventable or could be handled in other ambulatory care settings. This list can serve as a launching point for teams brainstorming diseases to target.
Building an LLM-first solution from the ground up for the right diseases (e.g. high cost and high unnecessary healthcare utilization) and modeled after gold standard existing startups such as Hinge Health could allow for very significant impact at attractive operational efficiencies.
Conclusion
In summary, here is the most promising startup opportunity we see for LLMs in this space:
Startup Opportunities:
Reducing ED Overutilization for Chronic Conditions: ambulatory sensitive conditions (ASCs) are treatable outside the hospital but often lead to unnecessary ED visits. Creating an LLM-first solution and targeting the right underserved ASC allows startups to compete in this space.
Intra-ED Triage and Patient Flow
Legend: ED = Emergency Department EMS = Emergency Medical Services RN = Registered Nurse NP = Nurse Practitioner PA = Physician Assistant DO = Doctor of Osteopathic Medicine ESI = Emergency Severity Index: ED triage algorithm from 1 (most urgent) to 5 (least urgent) Obs = Observation Unit *Emergency Medical Services Arrivals, Admission Rates to the Emergency Department Analyzed
A Walk Through the Process Map: Pain Points, Current Solutions, and LLM Use Cases
Intra-ED Triage
Triage is a critical ED workflow to ensure the right level of limited resources are allocated to the patients who need it most, to ensure patients continue to flow efficiently through the ED while minimizing bottlenecks, and to make the correct decisions regarding the patient’s ultimate destination (e.g. anywhere from back home without any follow-up to the intensive care unit).
Most EDs use the Emergency Severity Index triage algorithm to allocate patients to the appropriate ED pathways. The scale ranges from 1 (most urgent) to 5 (least urgent). Identifying the sickest (1) and least sick (5) patients is typically not as difficult as parsing the more intermediate scores of 2-4. For example, some of the patients initially placed in the 2 bucket may actually belong in the more severe 1 bucket, while some of the 3s and 4s may actually be lower-risk and good fits for a fast track to discharge from the ED.
This is what startup Stochastic (acquired by Beckman Coulter) focuses on. They provide a clinical decision support tool that uses “traditional” AI to recommend the appropriate ESI which allows them to reduce the time needed to make two very important decisions in the ED: who to admit and who to escalate to emergent care.
There is already academic evidence that LLMs could also be used successfully for ED triage. A recent cross-sectional study of over 250,000 adult ED visits at UCSF investigated the potential for an LLM to classify acuity levels. The LLM demonstrated accuracy of 89% and was comparable with human physician classification.
Mednition is another startup that provides ED triage tools for the general patient population like Stochastic while also offering tailored tools for a specific high-risk ED population, patients with sepsis (i.e. a severe bloodstream infection). Its tool for the general ED population provides real-time clinical risk guidance for emergency nurses to reveal hidden risk and prompt early intervention. Its sepsis AI solution uses multimodal data from the EMR to identify patients with sepsis earlier, which is critical because sepsis is the #1 cause of hospital death and nearly 6 in 10 patients with sepsis are missed during triage screening.
Patient Flow
While triage is critically important in the ED, optimizing patient flow is also critical. After all, if bottlenecks accumulate, the ED gets backed up, capacity gets overwhelmed, and critically sick patients can be missed or receive dangerously delayed care.
Several companies have attempted to address this by creating “command center” style solutions. Qventus is one such startup. They use AI and other analytics techniques to optimize throughput, predict and avoid crowding, and match staffing to demand. This results in decreased time spent by patients before being discharged, reduced time until a patient first sees a provider, and a reduction in patients who leave before seeing a provider. One constraint on improved flow in the ED is inpatient (hospital) flow, which Qventus also provides solutions for.
One significant barrier to fully optimizing patient flow is that clinical endpoints are often the prime determining factors and rate-limiting steps for a patient's ultimate destination (e.g. back home, hospital, ICU). For example, there are often very algorithmic, guideline-based, and essentially required tests and interventions that must be completed for patients with certain conditions to be safely triaged (e.g. a patient presenting with chest pain).
Synergizing Triage and Patient Flow via Optimized Clinical Endpoints
Two unicorn startups, Viz.ai and Heartflow, have done a great job of innovating around clinical endpoints to significantly improve patient triage and flow for their target patient populations.
For example, Viz.ai uses an AI-powered care coordination platform to analyze medical imaging data, including CT scans, EKGs, echocardiograms and more, to provide real-time insights and automated assessments to accelerate diagnosis and treatment. For example, their platform was associated with a nearly 40 minute reduction in patient arrival to the time of first contact with needed emergency stroke treatments. They have since expanded to develop similar products for other neurologic, vascular, and cardiac conditions.
Viz.ai’s key innovation was using ML to increase the speed and accuracy of a key clinical endpoint (imaging) to unlock much faster and safer triage and patient flow for their target patients.
“Initially, our focus was on deep learning for interpreting image-based data like CT scans, ECGs, and echocardiograms. We believe there is huge synergistic potential in merging traditional AI, like deep learning, with generative AI. This combination can address two major challenges. First, we noticed a significant gap in appropriate patient follow-up and disease missed due to unlinked clinical notes in EHRs. Important patient details often remain isolated, not contributing to subsequent, clinical guideline recommended care steps. Second, we observed that care teams, including ER and trauma doctors, who deal with a wide range of cases, struggle with extensive, ever-changing clinical guidelines that are already challenging enough for subspecialists to keep up with in their much narrower fields.
To tackle these issues, we're enhancing our pipeline to integrate deep learning image analysis with LLM-based synthesis of EHR data. This will enable our Viz.ai One Platform to then provide relevant clinical guidelines tailored to each patient, facilitating better care coordination. We believe this approach is crucial for reducing care variability and improving access to quality healthcare, especially in underserved communities. When we take generative AI and marry it with our well-validated traditional AI, we are able to create something truly powerful for healthcare providers, life science companies, and patients.” — Jieun Choe, Chief Marketing Officer of Viz.ai.
Heartflow is another unicorn startup using technology in innovative ways to more effectively triage patients in the ED. They developed AI algorithms coupled with CT imaging of the arteries of the heart, which allow for noninvasive assessment of the blood flow supplying the heart, reducing the need for invasive heart catheterizations. The most recent cardiology guidelines strongly advocate for the first-line use of their technology in low to intermediate risk acute chest pain patients allowing for faster and safer discharge of these patients from the ED, some of whom might otherwise have been admitted to the hospital.
Guideline-based care, prioritization, and bed flow
We already see Mednition, Viz.ai and Heartflow very focused on improving ED patient triage and flow via optimizing clinical endpoints for very specific patient populations (e.g. sepsis, stroke, chest pain), but what if a startup could develop a general command center for the ED for the most common presenting complaints? LLMs could analyze each patient’s history, compare it to their presenting complaint, and track the evolving progress of their ED journey against the current guidelines of care. For example, there could be estimated progress bars next to each patient with certain patients flagged because the only thing preventing their discharge is an imaging study or repeat lab which has not been ordered despite the patient sitting idle for an hour.
While command center software has been developed by several companies for the ED, this is often more focused on operations (e.g. bed management and staffing) at a much higher level. A patient-by-patient focus at the clinical level (now enabled by LLMs) would provide unique value for enhancing patient flow.
Guiding Patients Through Their ED Journey
Digital patient engagement remains a significant challenge in EDs. A 2024 study of 1.28 million ED visits found that only 17.4% of patients used patient portals during their visit, with significantly lower usage among male patients, Black patients, and those without commercial insurance. Patients with active portal accounts at ED arrival had significantly higher odds of using the portal—approximately 17 to 18 times greater—compared to those without active accounts, highlighting the importance of pre-visit digital engagement.
Some startups like Fabric (formerly Florence) are working to address this gap by engaging patients before they even walk into the ED.
Fabric provides a mobile app that provides several services: 1) it allows patients to initiate the registration process before arrival or while awaiting care, 2) it provides a map of the patient’s journey and their visit progress which reduces the likelihood of patients leaving without being seen, 3) it provides a digitized rapid assessment tool to quickly assess acuity, offers clinical decision support to providers, and appends this data to the EMR with adaptive patient interviews reducing documentation burden, 4) it allows for digital discharge avoiding the need for paperwork, and 5) it provides tools to schedule follow-up appointments.
Triage + Patient Navigation Agents
We see an interesting opportunity to create an LLM-native solution to take triage and patient navigation to the next level.
For example, on the way to the ED, patients would interact with chat and / or conversational AI agents, which would seek out patient history and reason for presentation. This could help triage patients more rapidly and, for lower acuity patients who face longer wait times to be seen, it allows them to stay engaged and essentially pre-populate the ED provider’s note, reducing documentation time and burden.
These agents could also gather information about social health determinants, conduct screenings for domestic violence and substance abuse, and guide patients throughout their ED care journey via real-time communication summarizing and explaining concepts in relatable terms all of which reduce nursing workload amidst growing shortages.
Conclusion
In summary, here are the most promising startup opportunities we see for LLMs in this space:
Startup Opportunities:
Guideline-based care, prioritization, and bed flow: LLMs to track patient courses and ensure faster delivery of guideline-based care for severe patients and those who could qualify for expedited discharges.
Triage + Patient navigation agents: LLM agents to gather history, triage patients, automate documentation, and guide patients through their ED journey via real-time communication summarizing and explaining concepts in relatable terms.
The views expressed herein are solely the views of the author(s) and are not necessarily the views of Maverick Capital, Ltd. or any of its affiliates. This article is not intended to provide, and should not be relied upon for, investment advice.